The Neonatal Neuro-Critical Care Program under the umbrella of the ACH Neuro-Critical care Program has developed an innovation in Neonatal Neuro-Critical Care Education Lab. The lab has produced (all developed locally) cutting edge innovative simulators and models that have been used across the globe for clinical care application, quality improvement and research.
Cranial Ultrasound Simulation Model:
Computer-Based and Brain Phantoms:
This was developed initially in collaboration with the sonographic Clinical Assessment of the Newborn Program.
The cranial ultrasound simulators allow learners to learn and practice ultrasonography using a bank of images obtained from patients with normal cranial structures and multiple pathologies, and ultrasound-able 3D printed heads with landmark brain structures. The preloaded images can be selected using the computer program, while the mannequin with sensors embedded under the scalp, allows the probe to select corresponding image sequences to simulate real life scanning. The components include a laptop computer connected to a sensor within the probe. The purpose of these tools is to familiarize trainees with probe orientation, image optimization skills and ultrasound machine knobology.
The Cranial Ultrasound simulator was developed at the University of Calgary by the Neuro-Critical Care Program based at the Alberta Children’s Hospital in partnership with the SCAN group.
Brain Phantoms
Ultrasound-able 3D printed heads with simplified key internal brain structures (lateral ventricles, caudo-thalamic notch and choroid plexus).
Computer-Based Cranial Ultrasound Simulators
- 3D printed heads with pressure sensors at the locations of the anterior and mastoid fontanels.
- 3D printed probes with Arduino sensors inside them to interact with the sensors in the 3D printed heads.

- Cranial ultrasonography software translates probe movements into images in a way that simulates a cranial ultrasonography study.

Implementation of The Models:
- The models have been used through conferences and hands-on workshops in several countries around the world (India, China, US, UK, Kuwait, Oman, Columbia and Quito) with more 1000 participants in total. We followed up with the centres after conferences and workshops organized by our group to help them build their programs and sustain the learned skills.
Clinical Skills and Education:
- The simulators have been integrated into our neonatology fellowship program. Currently all of our neonatology fellows get trained in neonatal cranial ultrasonography, compared to no training before we developed the models.

Quality improvement:
- The models have been used as a tool to standardize preterm brain injury definition by radiologists and neonatologists: two workshops were conducted in Calgary and Toronto with representatives from radiology and neonatology from each level-three centre in the country. The core group has become a taskforce which since created a consensus practice guideline to standardize the diagnosis and imaging in preterm infants across the country.
Research:
- We used the model in testing the efficacy of simulation-based learning in gaining and sustaining ultrasonography skills. We published the results in a peer reviewed journal.
- In the development, is a smart tracing of the lateral ventricle borders to measure surface area to compare it with traditional 2D measurements to better predict the ideal time for surgical intervention.
- MRI cases side by side to the same US pathology to be sliced simultaneously while performing cranial ultrasound
- Create interactive interface (quizzes and labeled anatomy and pathology) to help trainees self-learn using the simulator
- Allowing physicians to add their own cases and create center specific libraries
- Brain phantoms with corpus callosum , cerebellum, and third ventricle
- Adding cerebral arteries doppler functionality
Cerebral Arteries Doppler Model:
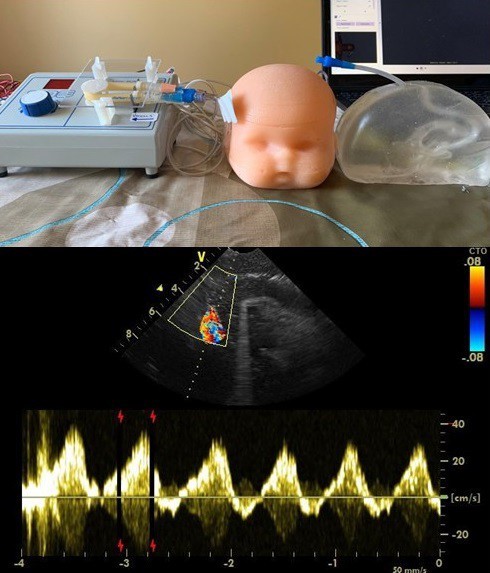
Anterior and Middle Cerebral Artery Simulator: This model features the anterior and middle cerebral arteries embedded in a realistic, ultrasound-compatible brain phantom.
Anatomy Included: Anterior Cerebral Artery, Middle Cerebral Arteries, and Cerebral Peduncle.
Simulation Mechanism: A peristaltic pump generates flow, while a 20 cc syringe allows for manual control of pulsation.
-
Learning Objectives:
Implementation: This model has been utilized in training at international workshops.
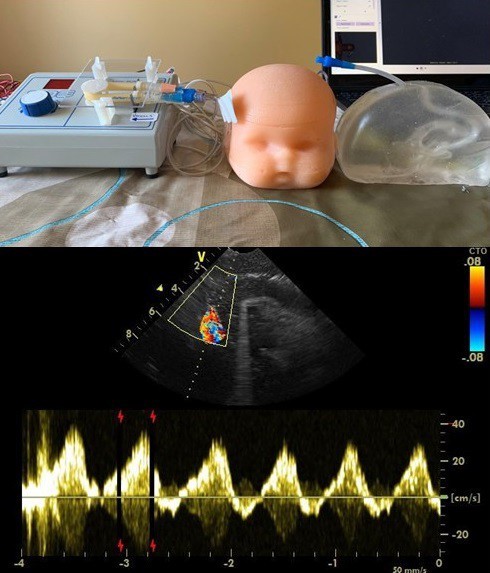
MCA model:

PHVD measurement and Reservoir Tapping Model:
As the surgical intervention for post hemorrhagic ventricular dilatation ( PHVD) is becoming rare, maintaining competency in taping the ventricular reservoir is a challenge. We developed a “just-in-time” teaching model which includes:
- Teaching Video
- Reservoir simulator: a reservoir was connected to an IV fluid bag embedded (hidden) in a mannequin body. A surgical incision and suture was created to resemble the real reservoir surgical site.
All in one
Implementation of the Model:
- The model is used as a “just in time” teaching tool each time we face a case of reservoir insertion.
- The model was used in international workshops such as Pediatric Academic Society and the American Academy of Pediatrics District VIII section of Neonatal- Perinatal Medicine.
Smart Phone Application for Preterm Brain Injury Diagnosis:
We converted the consensus view point that we developed between neonatology and Radiology into a smartphones application and made it free on google play and iPhone to improve compliance and decrease variability.
Preterm brain injury diagnostic tool on apple store
Preterm brain injury diagnostic tool on google play
Using AI , we developed all in one tool for GMH-IVH prevention, management and diagnosis.
NeuroSono - Preterm Brain Injury Consensus
Research:
Simulation-Based Structured Education Supports Focused Neonatal Cranial Ultrasound Training - PubMed
Neonatal Neurological Examination Teaching Simulators and Modules:
The purpose of these set of simulation models and teaching module was to improve identification of infants suffered from perinatal asphyxia and eligible for therapeutic hypothermia due to short window of opportunity to start the treatment
Targeted Neurological Examination Teaching Videos:
A formal consent was taking from families and full neurological examination videos were recorded for normal and abnormal newborns. The videos were then edited and integrated into one targeted neurological examination to improve HIE identification.
Therapeutic Hypothermia Smartphones Eligibility Tool:
Smart phones application was developed and made available for free to service as a checklist and decision making tool.
Targeted Neurological Examination Virtual Reality Module:
Recorded videos were converted in animation scenarios then used to create a virtual reality module in which trainees can observe and perform targeted neurological examination.
Neurological Examination Mannequins:
In collaboration with a group with computer science, mechanical engineers, and bioengineers, a neurological examination model was developed to simulate the tone assessment and posture.
The project won the best in clinical category at the 2019 health hack competition.
Clinical Skills and Education:
The combined package of teaching modules and simulators were used in the Southern Alberta Neonatal Outreach program where we vested all level I and II referring centres and conducted sessions on improving HIE identification.
The models were used at 2 workshops in Kuwait and Nursing neonatal Neuro-Critical care workshop in Calgary.
Impact:
After the implementation of theses teaching simulators and modules the rate of missed cases decrease significantly from 28% to 7% without increasing our total annual number.
Research:
The Utility of Simulation-Based Training in Teaching Frontline Providers Modified Sarnat Encephalopathy Examination: A Randomized Controlled Pilot Trial - PubMed
Using AI , we created all in one tool:
POLAR Protocol Navigator
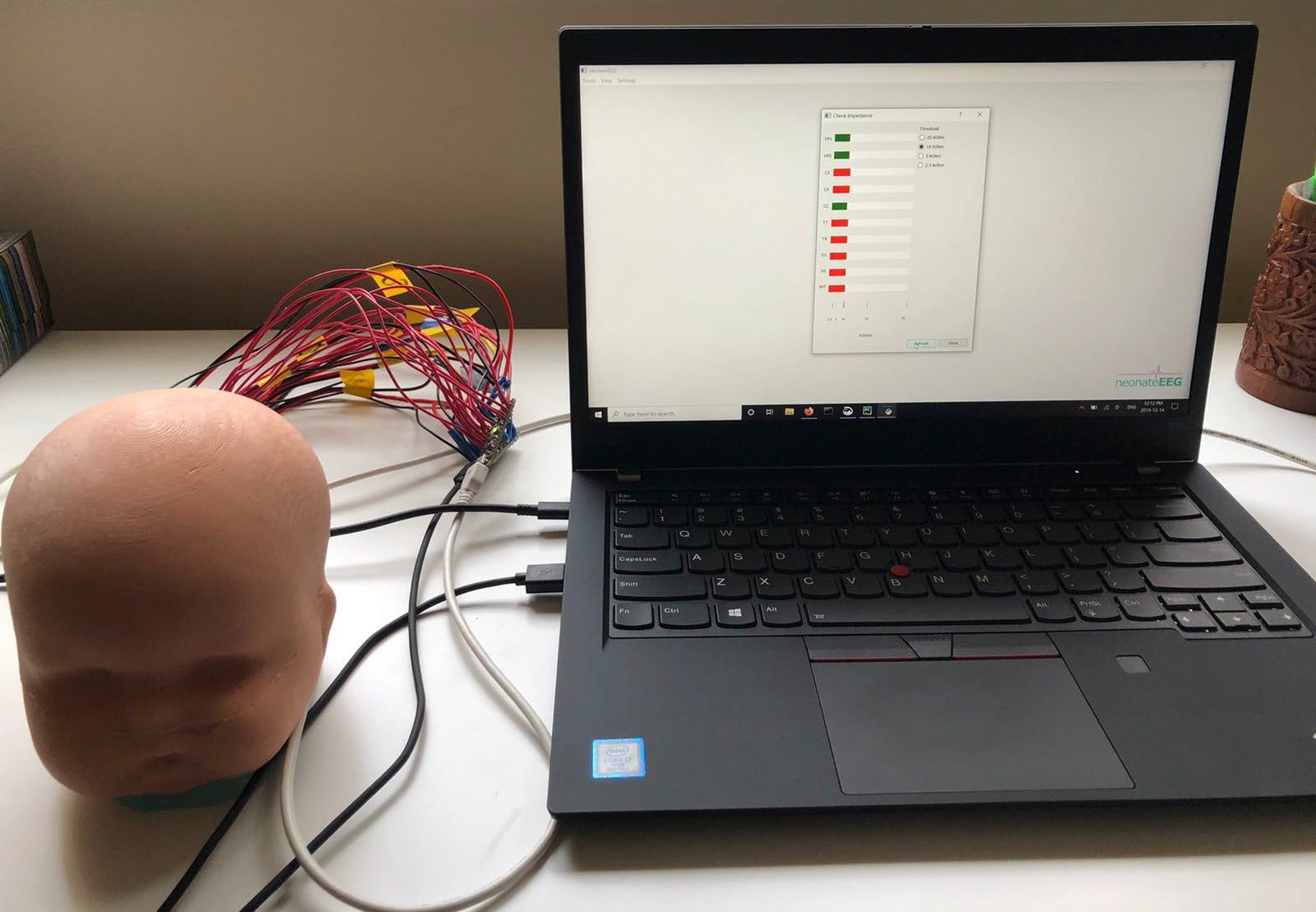
Neonatal Electro-Encephalogram (EEG) Teaching Modules and Simulator:
Teaching videos were created to demonstrate how to place EEG electrodes and generate a good quality signal with "step by step - how-to" tutorials on starting an EEG study and troubleshooting.
In collaboration with computer science, mechanical engineers, software engineers, and mechanical engineers an EEG simulator was developed to simulate EEG set up.

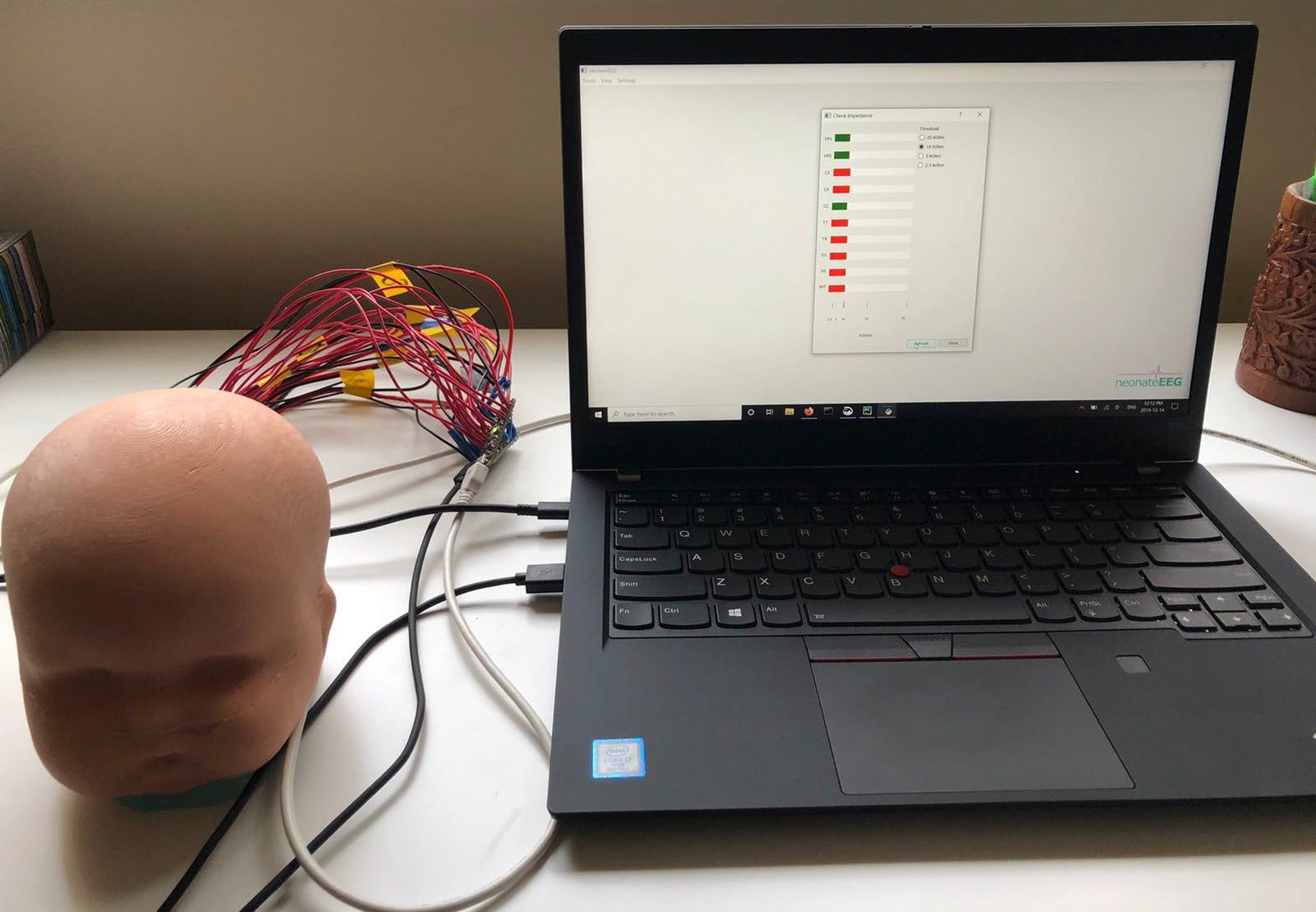
Clinical impact:
Using all teaching modules (teaching videos, documents, small group training, workshops, and recently the simulator) we trained NICU nurses to set up EEG studies which helped in the establishment of our neuro-monitoring in the NICU. Having NICU nurses initiate EEG studies significantly decreased time to initiate EEG studies. Establishing neuro-monitoring in the NICU resulted in significant reduction in anti-seizure medication use and improved seizure diagnosis.
Teaching EEG Set up Using Simulation and Live Children:
The EEG and neuro exam simulators were used at our local, national and international workshops with our own children volunteering as simulation models.

Using AI we created seizure diagnosis and management tool
N-SMART: Neonatal Seizure Management
NeoConvulse - Neonatal Seizure Guide